It's time to embrace some of the old-fashioned ways again![...]
Healthy Living
It's time to embrace some of the old-fashioned ways again![...]
Thoughts on love, selflessness, support, and sacrifice.[...]
How to use the positive feedback loop to create synergy and start[...]
I am not a personal trainer. These exercises are what I actually[...]
ANYONE can do a pushup by following this simple routine and practicing[...]
Subscribe To Our Newsletter!
Make sure to never miss a post by subscribing!
The Informed Patient
Watch and learn how you can prevent colon cancer![...]
Would you take fashion advice from a person still dressed in clothes[...]
A board-certified gastroenterologist shares 5 secret tips to make your colonoscopy prep[...]
How to tell if cannabis use is causing frequent vomiting attacks[...]
Every question you could ask about colonoscopy, answered![...]
Psychology And Motivation
My technique for avoiding the trap of false choices.[...]
Is your doctor really responsible for keeping you healthy? Who has the[...]
I'm willing to bet that most people's New Year's resolutions have something[...]
We all knew John was going to fail. His plan was barely[...]
It just so happens that this interaction occurred during a particularly low[...]
Gastroenterology And Endoscopy
An original article using statistics to more accurately predict the meaning of[...]
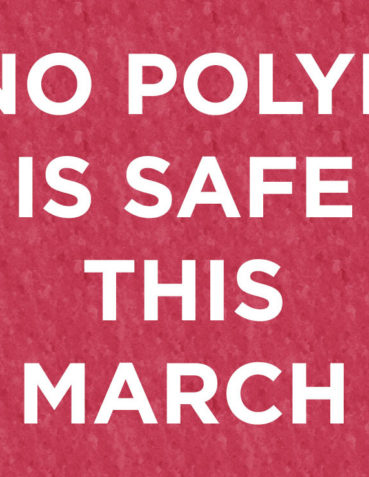
Colorectal Cancer Awareness Month continues on! However let’s face it, awareness by[...]
Now there is a new product called Eleview (Aries Pharmaceuticals) that is[...]
Why wouldn't a fellow endoscopist sent their patients for a procedure that[...]
MILAN, Italy: Gastroenterologists rejoice! Innuendo Technologies has announced that FDA approval of[...]
The Practice Of Medicine
What will it take to beat coronavirus?[...]
Why telemedicine, how to do it, and much more.[...]
It is estimated that 35-54% of doctors and nurses are burnt out.[...]
White coats should not be worn by physicians any longer, and should[...]
If you've ever thought about leaving your current job, this article is[...]
Subscribe To Our Newsletter!
Make sure to never miss a post by subscribing!