Over two years ago, I had a colon resection for the removal of a cancerous tumor (stage 2A). Ever since, I have had on and off bleeding in my stool. My surgeon has done two sigmoidoscopies and my gastro doctor has done two colonoscopies.
What is immediately apparent from these numbers is that Cologuard rarely misses cancer. However, if we count polyps as a significant finding, there are plenty of false-positive results (45%) and plenty of false-negatives too (34%). So is Cologuard a good test overall?
One useful technique to minimize the risk of perforation when treating large angiodysplastic lesions (let's arbitrarily define large as greater than 10-mm in diameter) is to...
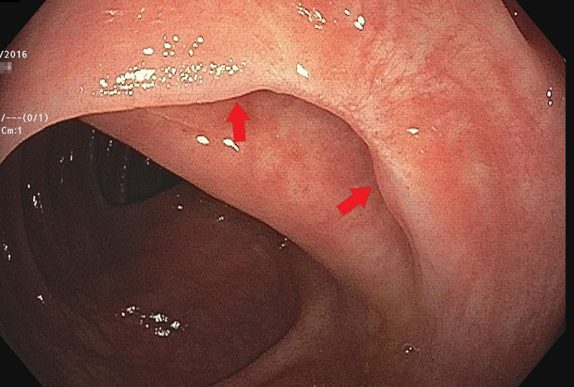
Should retroflexion in the right colon become a routine part of screening colonoscopy? Let's frame this question with the following facts: Colonoscopy is less-protective against right-sided cancers (which implies that colonoscopy is less-effective at finding or removing right-sided polyps...
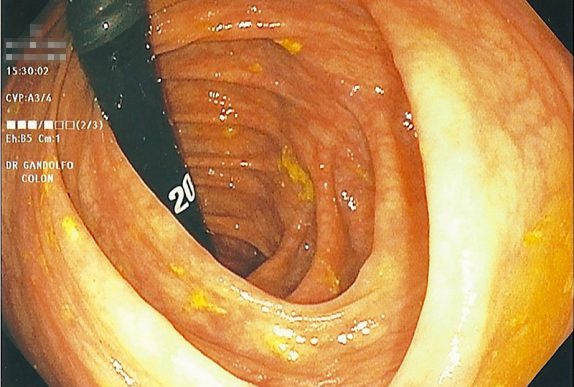
Since the name of my site is Retroflexions, it's about time I wrote an article about how to retroflex! More specifically, how does one retroflex in the right colon? (Fair warning: This article is probably only interesting to gastroenterologists.)
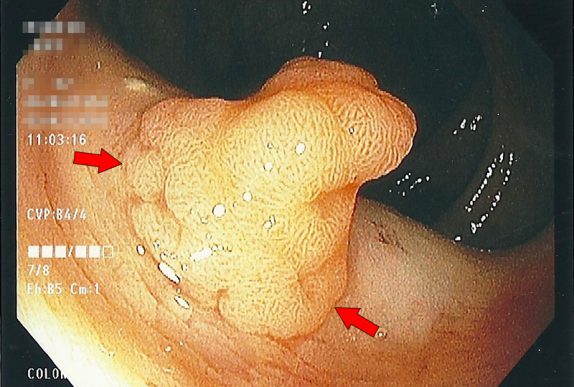
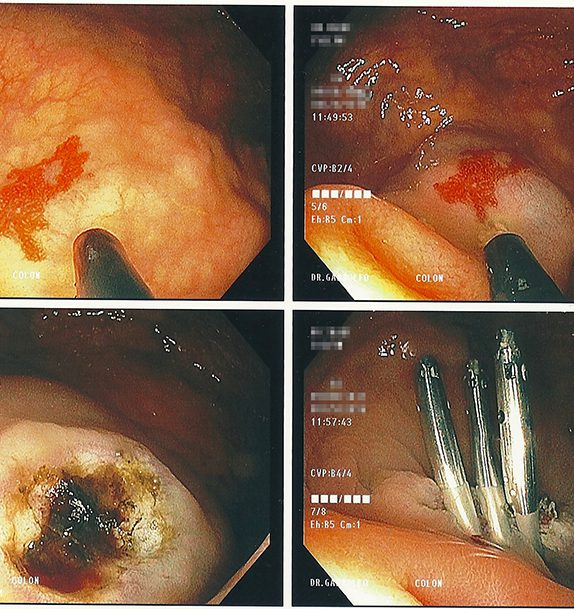
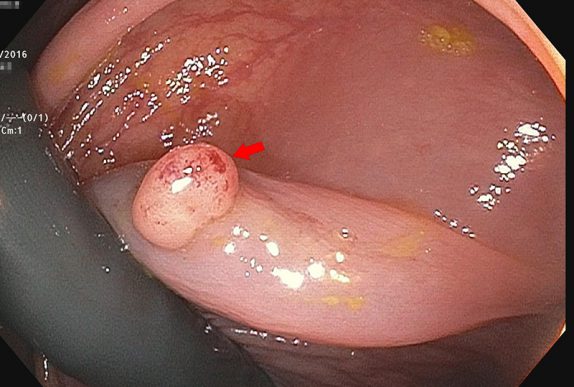
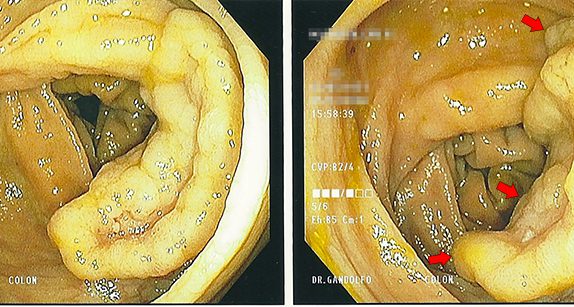
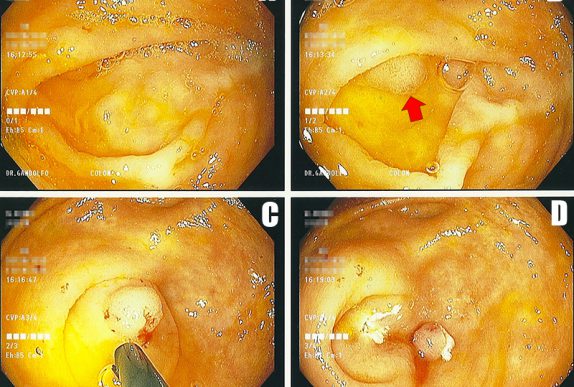
After removing a large polyp endoscopically, it is recommended to follow up the site about 3-6 months later to make sure the entire lesion was removed and prove there is no further adenomatous tissue to resect.
Sometimes repositioning the lesion is what it takes to get it done. A better angle between the snare and the polyp can be the difference between sliding over the top or capturing the lesion. In this case, retroflexing the scope in the ascending colon was the key maneuver needed to get the rest of the polyp out.
In keeping with the theme of women being smarter than men, the authors found no association between the happiness of the marriage or the degree of support from their husbands for women who chose to get a colonoscopy. Basically, women are just better at taking care of themselves independently without the need for their husbands approval, input, or coercion.
With all this talk about bleeding, it should come as no surprise that "Should I stop my aspirin?" is one of the more common questions that I get asked by patients who are being seen to arrange screening colonoscopy. Luckily, this question has been answered already by several of the gastroenterology societies. For the average patient on aspirin...
If you notice, the basic idea here is pretty simple. According to the guidelines, there are really only a few options for follow-up intervals for colonoscopy: 10 years (negative exam), 5 years (low risk polyps), and 3 years (high risk polyps). Less than 3 years is only recommended in the truly unusual case of a large polyp burden or invasive cancer in a polyp. And that's it.
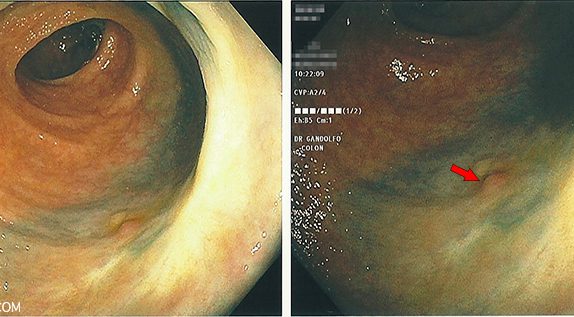
I thought it would be a good time to show a real-life example of colorectal cancer prevention in action. Let's pretend that you are a friendly neighborhood gastroenterologist, just minding your own business and doing a screening colonoscopy on a patient.
It is sometimes an awkward conversation to have, but the truth is that at a certain age, we eventually stop checking people for things that may cause them future harm.
Clearly, the screening guidelines recommend repeating a negative colonoscopy in ten years. Now what if I told you that many (if not most) practicing gastroenterologists recommend repeating the test in five years, not ten?
If there is one take-home message for colorectal cancer screening it is this: Start screening most people at age 50. Colonoscopy is the preferred screening test.
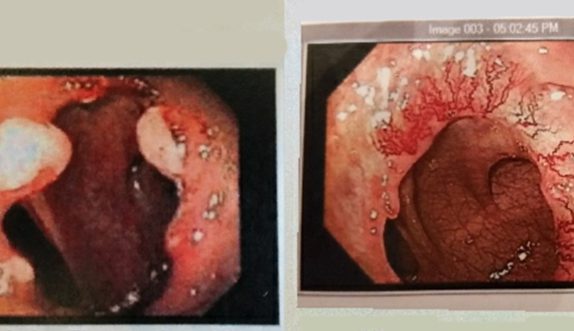
Three month follow up after removal of a small colon tumor with colonoscopy. Did the resection work, or did the patient ultimately need surgery?