Here in Long Island, NY where I practice, it seems to be the norm to have a precolonoscopy visit. This visit serves several important purposes in my mind: I can meet the patient, take a history, and make sure they actually need a screening colonoscopy. I can answer all of the above questions in more detail than the primary doctor can. I also get to give them my basic talk about the purpose of a colonoscopy, how and why we remove polyps, the importance of good bowel prep and how to do it, and the small associated risks of a colonoscopy. We can talk about what to do with medications, and where to arrive on the day of the test, and parking, and all those seemingly small details that can make a patient stressed-out about the test for no good reason.
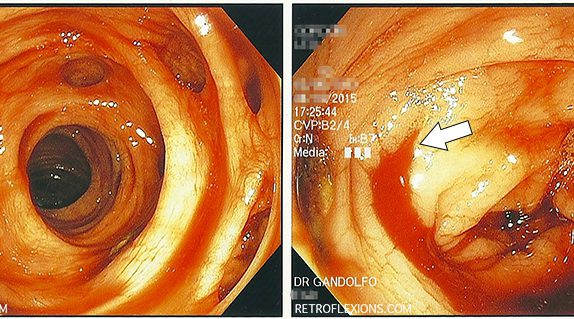
Knowing your limits is a very important part of doctoring. As Mark Twain said, "Good decisions come from experience. Experience comes from making bad decisions." Tackling big polyps with the scope is no exception to this rule. Although techniques for removing large polyps have evolved over the years, and maneuvers that were once deemed "high-risk" are now being taught fairly routinely to junior GI fellows, there is still an individual comfort level that practitioners should identify in themselves and respect.
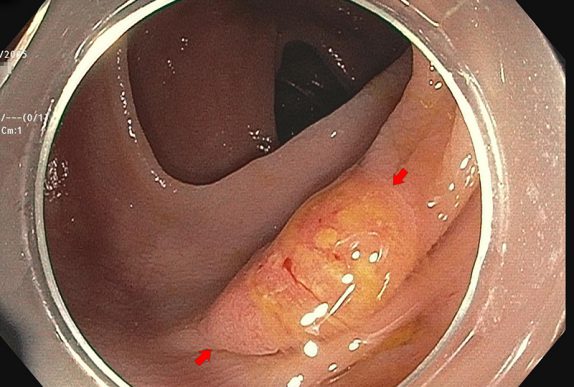
It is common practice to leave a permanent tattoo at the site of significant pathology ( such as a large polyp or tumor) inside the GI tract. We typically use a substance called SPOT, which consists of microscopic carbon particles in a suspension. When injected into tissue it becomes a permanent mark that can be seen from the inside of the organ with the scope, and from the outside of the organ by a surgeon.
I was surprised when the pathologist called me a few days later about the patient, since pathologists usually only call when a result is malignant or unusual. This "polyp" which I estimated to be about 15-mm in greatest diameter was a serrated adenoma (not a surprise) but also contained an 8-mm focus of adenocarcinoma. Luckily, the carcinoma portion of the polyp was completely resected with clear margins on all sides, however this polyp was truly an early-stage colon cancer!
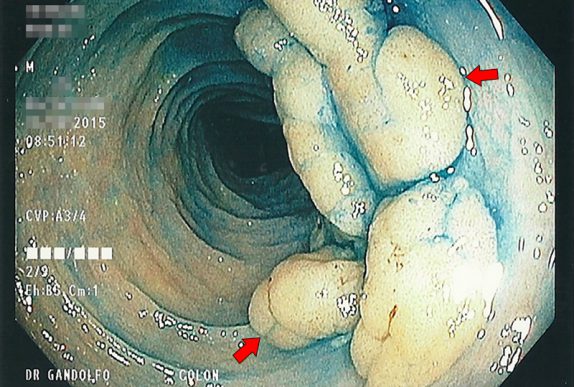
This lesion exhibits the "mucus cap" sign. There is a thick layer of mucus adherent to the polyp that remains attached even after washing with the water jet on the scope. The mucus cap sign is often seen with a particular type of polyp called a serrated polyp. These are often located in the right side of the colon, and are thought to be easier to miss on colonoscopy due to the flat nature of their growth. Unfortunately, they can still transform into colon cancer.
For many years, the effect of NSAIDs on preventing colon cancer has been described. There are numerous studies showing a small but mostly consistent decrease in both the development of polyps, and the development of colorectal cancer with chronic NSAID use. However, thus far there has not been a recommendation to take NSAIDs specifically with the goal of reducing the development of colon cancer, since the risk of chronic NSAID use is thought to outweigh any benefit in cancer prevention.
Overtesting and over treatment are big problems in modern medicine. It sometimes goes like this: Have a minor complaint? It's probably nothing, but we should do an exhaustive workup because there is a 0.00001% chance it could be cancer, maybe. However,
Is this common practice of bridging from Coumadin to an injectable anticoagulant back to Coumadin necessary? From a practical point, it is usually a major inconvenience for patients and doctors alike. Many patients are uncomfortable giving themselves injections at home. The injectable anticoagulants are sometimes expensive. Sometimes despite good instruction, they are administered incorrectly by the patient, or on the wrong dates. What if Coumadin was just held and later restarted without the bridging?
(Don't click if you don't want to see blood!) Diverticular bleeding can happen without warning, and is painless. A large volume of bright red or sometimes dark red blood per rectum is often the only symptom. In most patients who are not on blood thinners, diverticular bleeding eventually stops by itself.
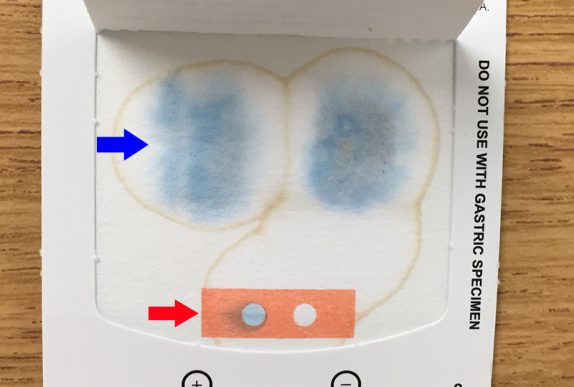
This will just be a cookbook-style post on how we do fecal microbiota transplant with colonoscopy. First, a healthy donor must be identified. The donor should be in good general health, since theoretically some problems such as obesity, diabetes, autoimmune disease, etc., may be transmitted by fecal transplant.
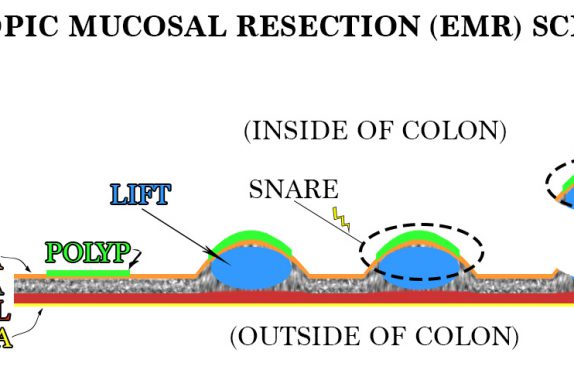
Many lesions that have been deemed "not endoscopically resectable" can actually be safely removed by a gastroenterologist with training and experience in EMR.
Of the cancers that both men and women can get, colon cancer is the second leading cause of cancer death in the Unites States. Colonoscopy, when performed by an expert with an adequate adenoma detection rate, has been shown to reduce the risk of developing colorectal cancer. For most people, routine screening colonoscopy is recommended starting at … Read more
Occult gastrointestinal bleeding simply means that there is blood loss into the GI tract that cannot be seen with the naked eye (as opposed to overt GI bleeding, where blood is seen). Typically, patients with occult GI bleeding have slowly progressive anemia due to slow chronic blood loss. There are a variety of causes of … Read more
The adenoma detection rate (ADR) is currently the best "report card" for colonoscopy performance available. All doctors that perform colonoscopy are not equally good at it. All endoscopists should be measuring their own individual ADR, and working to push that number higher and higher.
As a patient, you only have control over a few parts of your colonoscopy. Usually you have a choice of which doctor does the procedure. You have a choice of showing up on the day of the procedure vs. running in the other direction. And finally, you have control on how well you are “prepped” … Read more