Here in Long Island, NY where I practice, it seems to be the norm to have a precolonoscopy visit. This visit serves several important purposes in my mind: I can meet the patient, take a history, and make sure they actually need a screening colonoscopy. I can answer all of the above questions in more detail than the primary doctor can. I also get to give them my basic talk about the purpose of a colonoscopy, how and why we remove polyps, the importance of good bowel prep and how to do it, and the small associated risks of a colonoscopy. We can talk about what to do with medications, and where to arrive on the day of the test, and parking, and all those seemingly small details that can make a patient stressed-out about the test for no good reason.
Dr. Gandolfo is a board-certified gastroenterologist in Long Island, NY. He is the founder of Retroflexions.com and enjoys writing about healthy living and the practice of medicine. He started his solo practice, Precision Digestive Care, in 2018.
Posts by Frederick Gandolfo, MD
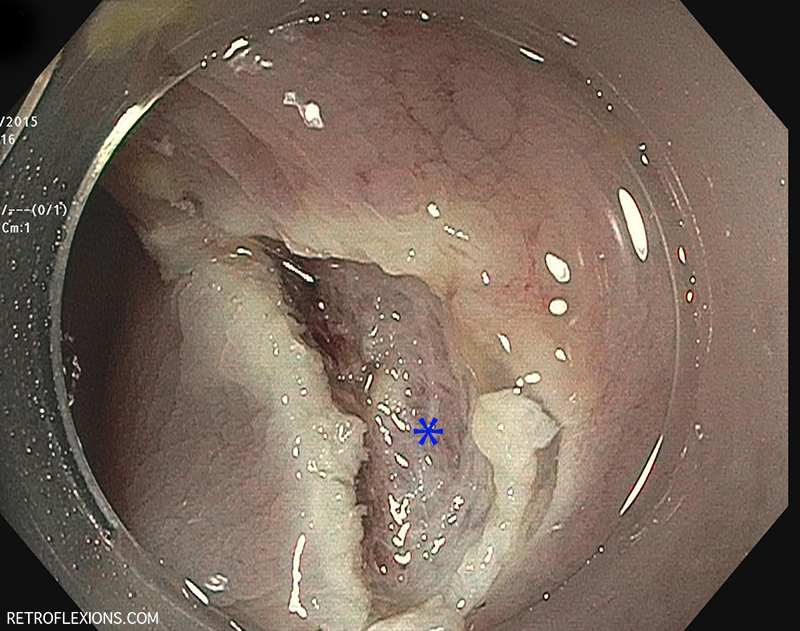
Knowing your limits is a very important part of doctoring. As Mark Twain said, "Good decisions come from experience. Experience comes from making bad decisions." Tackling big polyps with the scope is no exception to this rule. Although techniques for removing large polyps have evolved over the years, and maneuvers that were once deemed "high-risk" are now being taught fairly routinely to junior GI fellows, there is still an individual comfort level that practitioners should identify in themselves and respect.
In every hospital I have ever worked in, from medical school to present day, there is a noise pollution problem of epic proportions. Every medical device seems to emit at least three different types of beeps, each of them being more loud and annoying than the next.
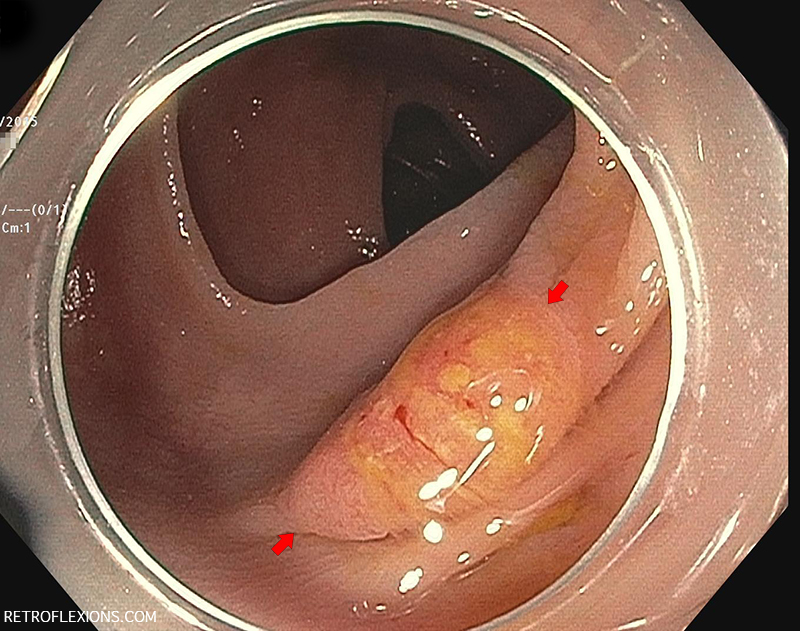
It is common practice to leave a permanent tattoo at the site of significant pathology ( such as a large polyp or tumor) inside the GI tract. We typically use a substance called SPOT, which consists of microscopic carbon particles in a suspension. When injected into tissue it becomes a permanent mark that can be seen from the inside of the organ with the scope, and from the outside of the organ by a surgeon.
I was surprised when the pathologist called me a few days later about the patient, since pathologists usually only call when a result is malignant or unusual. This "polyp" which I estimated to be about 15-mm in greatest diameter was a serrated adenoma (not a surprise) but also contained an 8-mm focus of adenocarcinoma. Luckily, the carcinoma portion of the polyp was completely resected with clear margins on all sides, however this polyp was truly an early-stage colon cancer!
Food impaction in the esophagus is one of the emergency conditions that only gastroenterologists and emergency room doctors know about. The overall concept is simple: Soon-to-be patient eats a large quantity of food (most commonly meat), which gets stuck in the esophagus somewhere and then causes a blockage and prevents further swallowing. Patient experiences chest pain, … Read more
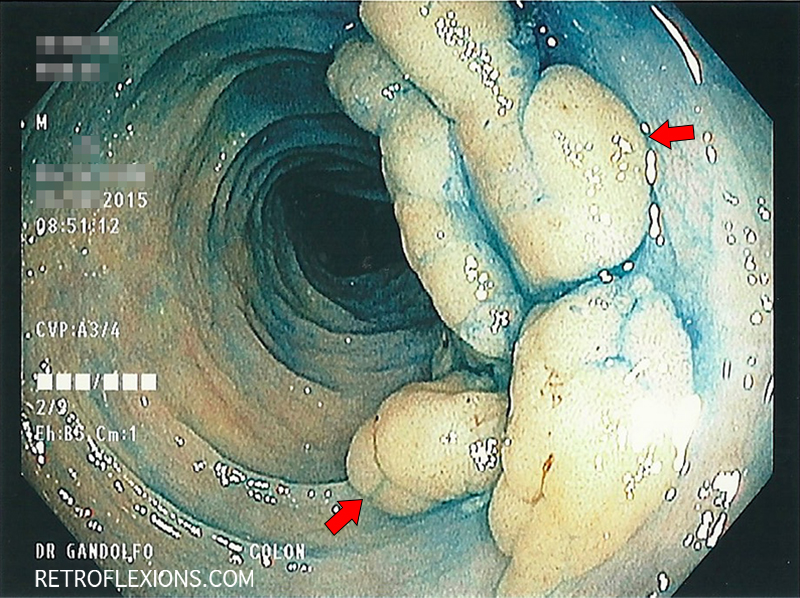
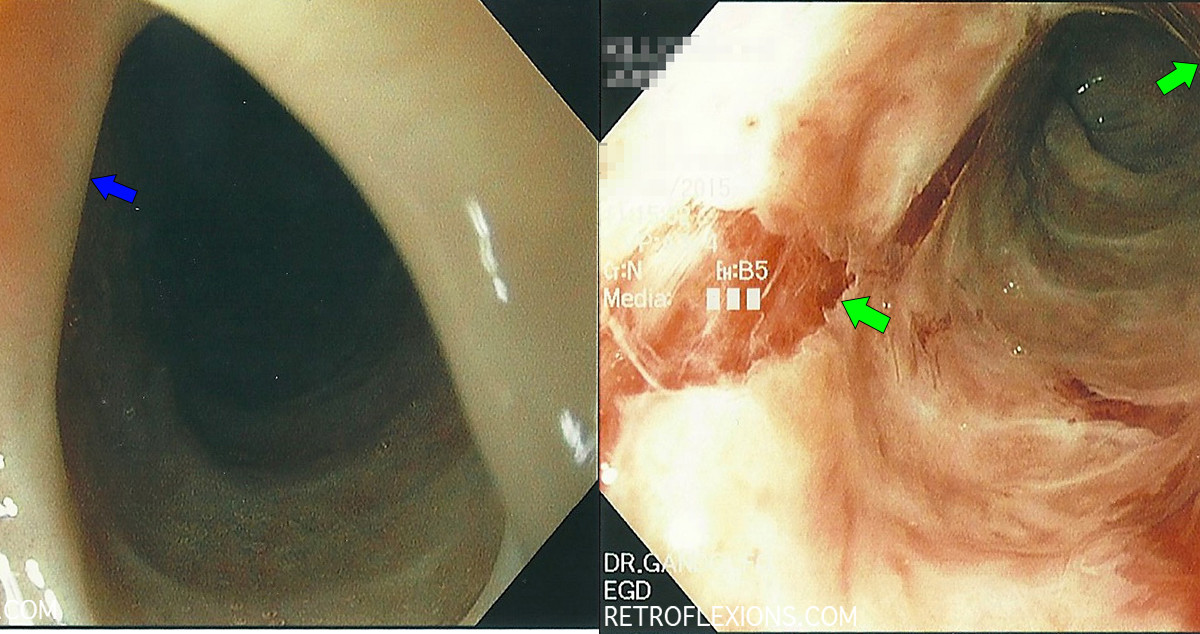
This lesion exhibits the "mucus cap" sign. There is a thick layer of mucus adherent to the polyp that remains attached even after washing with the water jet on the scope. The mucus cap sign is often seen with a particular type of polyp called a serrated polyp. These are often located in the right side of the colon, and are thought to be easier to miss on colonoscopy due to the flat nature of their growth. Unfortunately, they can still transform into colon cancer.
Dysphagia (trouble swallowing) can be caused by many different problems. A strictured or narrowed esophagus is one common cause, and is often related to excess acid exposure in the esophagus. Usually strictures happen at one discrete location in the esophagus (often the lower part closest to the stomach where acid reflux damage is the most pronounced).
So what does this all mean? Should you never eat red meat? Is this the end of the bacon cheeseburger? Of course not! When faced with information like this we really need to step back and look at the big picture. How much do you enjoy eating a juicy steak or a grilled hot dog on a warm summer day? What is the purpose of life? What is the lifetime mortality of someone who never eats red meat? (Hint: it's 100%.) Let's not forget that red meat is also an excellent source of protein, iron, B vitamins, and zinc...oh, and it tastes pretty good too!
So what are some take home points about meat intake in Crohn's disease? Red meat (beef, lamb, pork [yes pork too!]) can be though of as pro-inflammatory foods. It is reasonable to limit consumption of red meat to once or twice per week at most. Fish is probably a good alternative to red meat. These recommendations are based on very limited, low-quality data. Sometimes this is better than no data at all!
For many years, the effect of NSAIDs on preventing colon cancer has been described. There are numerous studies showing a small but mostly consistent decrease in both the development of polyps, and the development of colorectal cancer with chronic NSAID use. However, thus far there has not been a recommendation to take NSAIDs specifically with the goal of reducing the development of colon cancer, since the risk of chronic NSAID use is thought to outweigh any benefit in cancer prevention.
Overtesting and over treatment are big problems in modern medicine. It sometimes goes like this: Have a minor complaint? It's probably nothing, but we should do an exhaustive workup because there is a 0.00001% chance it could be cancer, maybe. However,
Most people know that they cannot eat anything after midnight if they have a procedure scheduled the next day. However, what about when a procedure is not actually scheduled? Sometimes a little bit of common sense and a little foresight needs to be applied to avoid having a procedure delayed an entire day because of the NPO rules. Here are two common situations that I encounter (without exaggeration) several times per week:
"Is it bad" is an honest question. "Is that bad" is usually also an honest question, but one that is much more difficult to answer. Patients usually ask "is that bad" without actually having a diagnosis yet. At the end of our visit I try to summarize the pertinent issues and I will usually list a few of the possible diagnoses that may explain the symptoms. Then we will come up with a plan to test for these diagnoses. I might say "This is probably irritable bowel syndrome, however some of the symptoms could be consistent with Crohn's disease or ulcerative colitis. We need to do further testing to figure out which one it is."
I call this the "Attribution Sign" and once you notice this is happening it is important to remain objective about the history and not fall into the trap that the patient is (inadvertently) setting for you. That is, don't place too much weight on the patient's attribution and don't let it skew your judgement.