It just so happens that this interaction occurred during a particularly low point of my fellowship, and I blurted out "Do you have...
Dr. Gandolfo is a board-certified gastroenterologist in Long Island, NY. He is the founder of Retroflexions.com and enjoys writing about healthy living and the practice of medicine. He started his solo practice, Precision Digestive Care, in 2018.
Posts by Frederick Gandolfo, MD
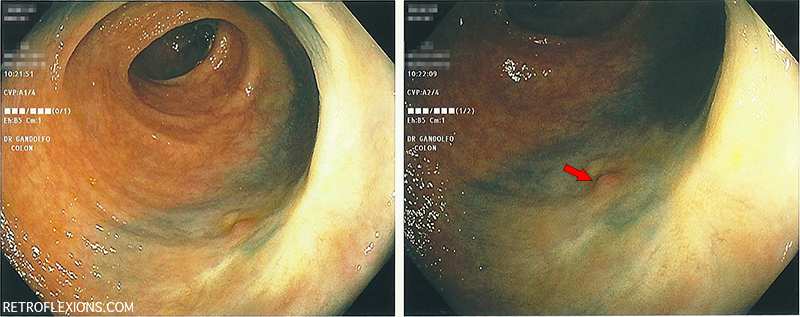
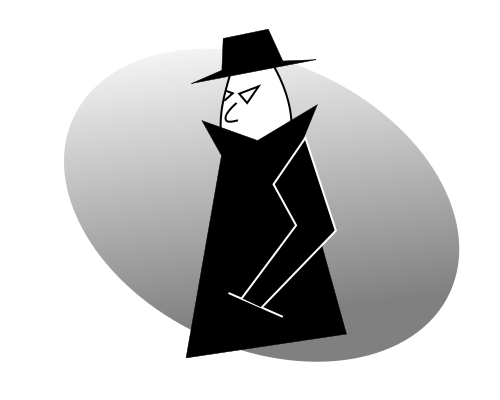
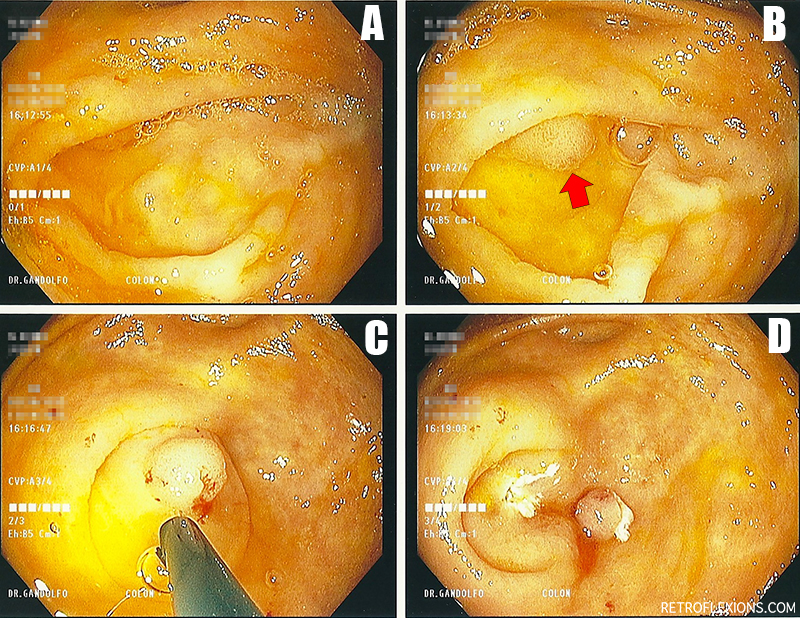
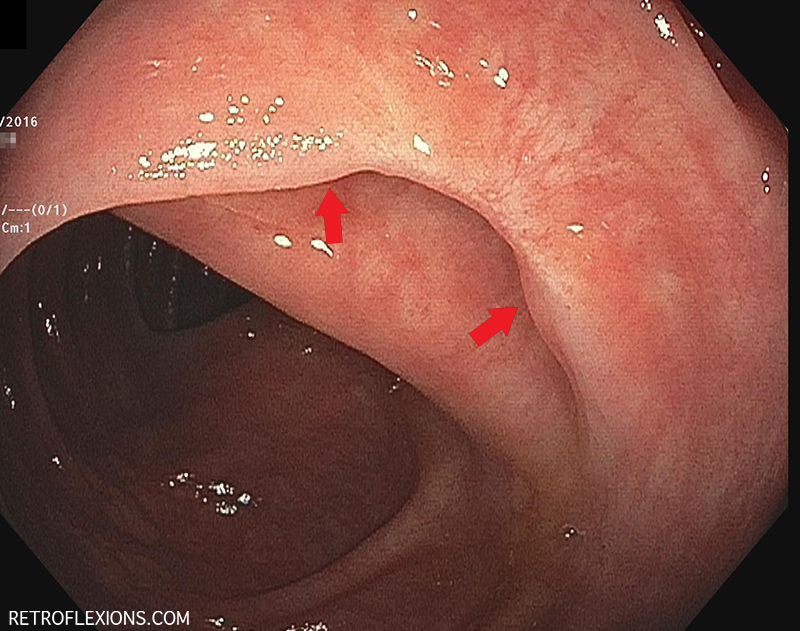
After removing a large polyp endoscopically, it is recommended to follow up the site about 3-6 months later to make sure the entire lesion was removed and prove there is no further adenomatous tissue to resect.
Sometimes repositioning the lesion is what it takes to get it done. A better angle between the snare and the polyp can be the difference between sliding over the top or capturing the lesion. In this case, retroflexing the scope in the ascending colon was the key maneuver needed to get the rest of the polyp out.
In keeping with the theme of women being smarter than men, the authors found no association between the happiness of the marriage or the degree of support from their husbands for women who chose to get a colonoscopy. Basically, women are just better at taking care of themselves independently without the need for their husbands approval, input, or coercion.
Now, I don't want to offend anyone with this post (it's already too late), but it seems these days that the only qualification that one needs to don a long white coat is to work in some patient care area of a hospital. The long white coat used to be the way patients, families, and other hospital medical staff could instantly tell who was a full-fledged attending physician. In fact, the emphasis on the white coat starts on the first day of medical school with something aptly called a "white coat ceremony."
With all this talk about bleeding, it should come as no surprise that "Should I stop my aspirin?" is one of the more common questions that I get asked by patients who are being seen to arrange screening colonoscopy. Luckily, this question has been answered already by several of the gastroenterology societies. For the average patient on aspirin...
Dear Retroflexions, As a victim of anal rape by my domestic married partner, I never recovered...
If you notice, the basic idea here is pretty simple. According to the guidelines, there are really only a few options for follow-up intervals for colonoscopy: 10 years (negative exam), 5 years (low risk polyps), and 3 years (high risk polyps). Less than 3 years is only recommended in the truly unusual case of a large polyp burden or invasive cancer in a polyp. And that's it.
I thought it would be a good time to show a real-life example of colorectal cancer prevention in action. Let's pretend that you are a friendly neighborhood gastroenterologist, just minding your own business and doing a screening colonoscopy on a patient.
It is sometimes an awkward conversation to have, but the truth is that at a certain age, we eventually stop checking people for things that may cause them future harm.
Clearly, the screening guidelines recommend repeating a negative colonoscopy in ten years. Now what if I told you that many (if not most) practicing gastroenterologists recommend repeating the test in five years, not ten?
If there is one take-home message for colorectal cancer screening it is this: Start screening most people at age 50. Colonoscopy is the preferred screening test.
If you are new to the site, I have basically tried to write about one short article per week about gastroenterology, medicine, doctoring, and other related topics.
Three month follow up after removal of a small colon tumor with colonoscopy. Did the resection work, or did the patient ultimately need surgery?
What is the deal with anal sex and fecal incontinence?