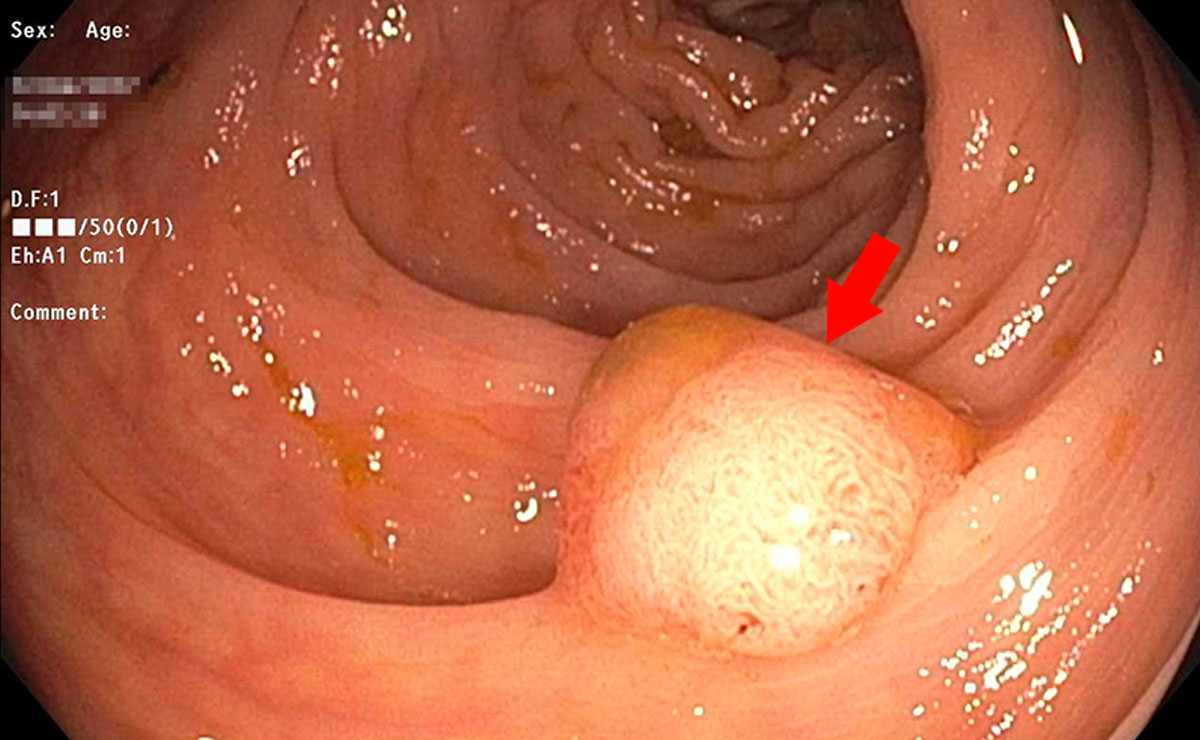
When it comes to colon cancer prevention, the polyp is the key player to know. Colon polyps, called adenomas, are precancerous growths originating from the inner lining of the colon wall. There are other types of polyps in the colon which are not considered precancerous, but for our purposes in this article we will consider the terms colon polyp and adenoma to be one and the same.
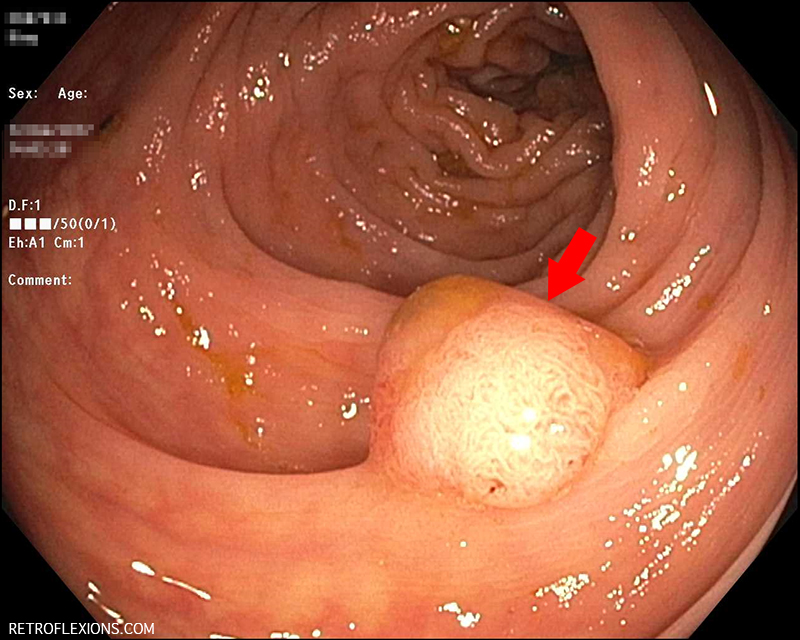
The red arrow is pointing to the adenomatous polyp. A polyp this size has a good chance of becoming cancer down the road if it is not removed.
Polyps are important to know about because they are the precursors to colon cancer. That is, virtually all cases of colon cancer began many years earlier as a small polyp growing in the colon. For the average person, it takes many years for these small polyps to appear on the scene, which is why we don’t usually recommend colonoscopy until a person is 50 years old. However, it’s not totally uncommon to find significant-sized polyps in younger people in their 30s or 40s (and even in their 20s!) From the time a polyp starts growing, it is thought to take more than 10 years for the polyp to grow into cancer…and not all adenomatous polyps grow larger or turn into cancer at all. However, many polyps will continue to have cellular changes such as mutations that will promote growth of the polyp and eventually transformation into colon cancer.
By understanding what causes colon polyps, we can understand what causes colon cancer. Here are some risks factors for getting colon cancer/polyps that an individual cannot change:
- Age: The risk tends to go up as one gets older.
- Sex: Men seem to have a slightly higher chance of having polyps when compared to women.
- Family history: A close relative with polyps or colon cancer makes your risk go higher.
- Race: Black men and women have the highest risk of developing colon cancer.
However, roughly half of all cases of colon cancer (and by extension, colon polyps) are a result of modifiable risk factors. These are the things that you can control. If we know what these risk factors are, maybe we can make better choices for ourselves and our families. The following is a list of the known risk factors for developing colon cancer/polyps:
- Alcohol: Alcohol use is closely tied to colon cancer risk. Unfortunately, even for “social” drinkers, the risk goes up by about 10% if you only drink less than 1 drink per day. If you have 2-4 drinks per day, the risk increases by 23%!

Alcohol use increases colon cancer risk.
- Red meat: Beef, veal, lamb and pork (despite the advertisements) are considered red meats. Regular consumption of about 100 grams of red meat per day (about the amount found in 2 regular-sized McDonald’s hamburgers) can increase the risk of colorectal cancer by 17%. I like the idea of “everything in moderation” so let’s aim to only eat red meat about once per week.
- Processed meat: This seems to be a real bad one…processed meat is often also red meat and is defined as meat that has been salted, cured, smoked, fermented, or treated with other processes to improve flavor or preserve the meat. Processed meat is bacon, sausages, hot dogs, cured ham, etc. The risk of colorectal cancer goes up by 18% for those who eat just 50 grams per day of processed meat (this is half the amount of red meat needed for the same risk).

A pile of processed meat. If this looks like your breakfast, you might have a problem!
- Lack of dietary fiber: Eating fiber is good for your colon for many reasons, and transmits a decreased risk of colon cancer as well. An extra 10 grams of fiber in the diet can drop colon cancer risk by 10%, but don’t stop there: Men should get 38 grams of fiber per day, and women are recommended to eat 25 grams per day. An apple has about 4 grams of fiber in it, so that’s a lot of apples to eat every day! Alternatively, you should eat a variety of plant-based foods and take in fiber with each meal and snack.

An apple has about 4 grams of fiber in it. Men, even if you eat all these apples in a day, you are still supposed to get in another 6 grams of fiber!
- Smoking: This seems obvious. Smoking causes all kinds of cancer. It also increases the risk of colon polyps and colorectal cancer. Smoking is not a great way to stay healthy.
- Obesity: Being overweight or obese increases the risk of colon cancer. This is independent of physical activity. That is, the excess weight itself seems to be tied to cancer risk, likely due to changes in inflammatory and growth signaling molecules, among other factors.
- Lack of exercise: Interestingly, staying physically active can reduce the risk of colon cancer by a whopping 25%! The minimum amount of exercise recommended for this purpose is about 2.5 hours per week of moderate exercise, or 75 minutes per week of intense exercise, but more is better. Again, the reasons for this are somewhat unclear but likely rooted in positive changes in insulin resistance, growth factors, inflammatory factors, and who knows what other things that are modified by exercise. We weren’t born to sit around, going from couch to car to chair and back again…we were born to move, so do something active on a regular basis!

You don’t have to run a marathon, but get out there and do something!
- Coffee: Well this should really read “lack of coffee” because coffee seems to be somewhat protective against developing polyps and colon cancer! There are not many high-quality studies on this topic, but what is out there suggests a 25% decrease in colorectal cancer with coffee consumption, possibly due to the antioxidants found in coffee.
- Calcium: This is controversial. On one hand it seems that high consumption of dairy products like milk is associated with a lower risk of colorectal cancer. At best, supplementing calcium seems to have no effect on cancer risk for better or worse. However a very recent study suggests an increased risk of adenomatous polyps from taking both calcium and vitamin D supplements in combination, so more research will be needed to figure out the exact role of calcium, vitamin D, and the combination of both for colon cancer prevention.
And let’s not forget the final factor that leads to colon polyps and cancer in many individuals:
- Bad luck: Unfortunately some people just have bad luck. We doctors don’t understand everything! This is why it’s still important to get screened for colorectal cancer at the appropriate age even if you don’t have any family history or symptoms, and are a thin, non-smoking, vegan, fitness-guru teetotaler!