With all this talk about bleeding, it should come as no surprise that "Should I stop my aspirin?" is one of the more common questions that I get asked by patients who are being seen to arrange screening colonoscopy. Luckily, this question has been answered already by several of the gastroenterology societies. For the average patient on aspirin...
If you notice, the basic idea here is pretty simple. According to the guidelines, there are really only a few options for follow-up intervals for colonoscopy: 10 years (negative exam), 5 years (low risk polyps), and 3 years (high risk polyps). Less than 3 years is only recommended in the truly unusual case of a large polyp burden or invasive cancer in a polyp. And that's it.
I thought it would be a good time to show a real-life example of colorectal cancer prevention in action. Let's pretend that you are a friendly neighborhood gastroenterologist, just minding your own business and doing a screening colonoscopy on a patient.
It is sometimes an awkward conversation to have, but the truth is that at a certain age, we eventually stop checking people for things that may cause them future harm.
Clearly, the screening guidelines recommend repeating a negative colonoscopy in ten years. Now what if I told you that many (if not most) practicing gastroenterologists recommend repeating the test in five years, not ten?
If there is one take-home message for colorectal cancer screening it is this: Start screening most people at age 50. Colonoscopy is the preferred screening test.
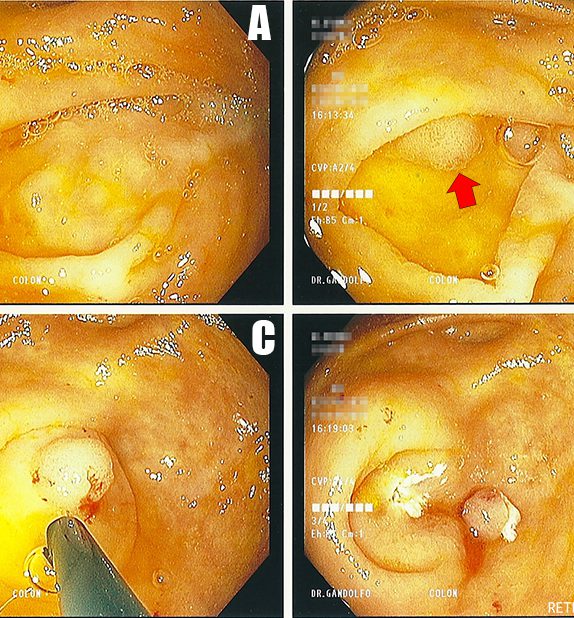
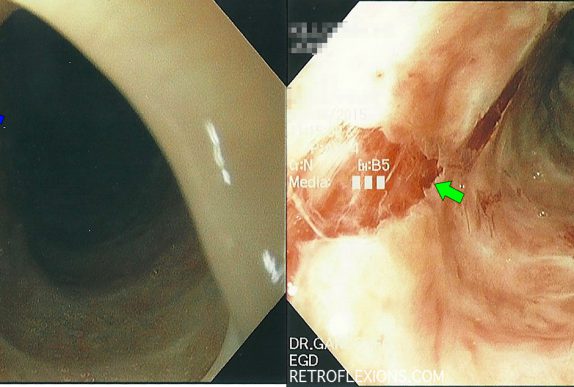
Three month follow up after removal of a small colon tumor with colonoscopy. Did the resection work, or did the patient ultimately need surgery?
Here in Long Island, NY where I practice, it seems to be the norm to have a precolonoscopy visit. This visit serves several important purposes in my mind: I can meet the patient, take a history, and make sure they actually need a screening colonoscopy. I can answer all of the above questions in more detail than the primary doctor can. I also get to give them my basic talk about the purpose of a colonoscopy, how and why we remove polyps, the importance of good bowel prep and how to do it, and the small associated risks of a colonoscopy. We can talk about what to do with medications, and where to arrive on the day of the test, and parking, and all those seemingly small details that can make a patient stressed-out about the test for no good reason.
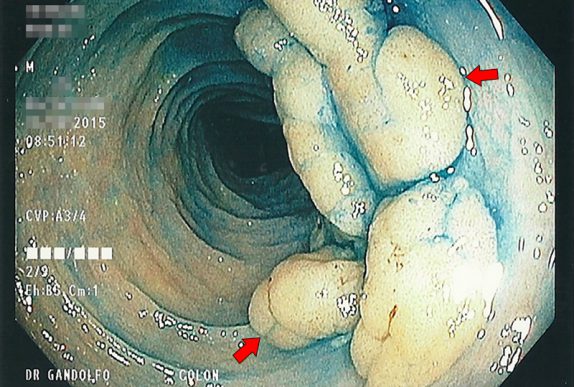
Knowing your limits is a very important part of doctoring. As Mark Twain said, "Good decisions come from experience. Experience comes from making bad decisions." Tackling big polyps with the scope is no exception to this rule. Although techniques for removing large polyps have evolved over the years, and maneuvers that were once deemed "high-risk" are now being taught fairly routinely to junior GI fellows, there is still an individual comfort level that practitioners should identify in themselves and respect.
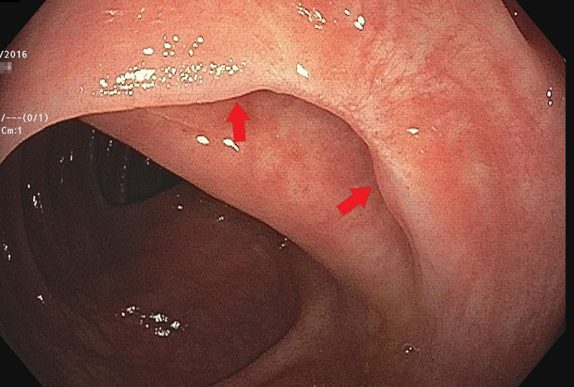
It is common practice to leave a permanent tattoo at the site of significant pathology ( such as a large polyp or tumor) inside the GI tract. We typically use a substance called SPOT, which consists of microscopic carbon particles in a suspension. When injected into tissue it becomes a permanent mark that can be seen from the inside of the organ with the scope, and from the outside of the organ by a surgeon.
I was surprised when the pathologist called me a few days later about the patient, since pathologists usually only call when a result is malignant or unusual. This "polyp" which I estimated to be about 15-mm in greatest diameter was a serrated adenoma (not a surprise) but also contained an 8-mm focus of adenocarcinoma. Luckily, the carcinoma portion of the polyp was completely resected with clear margins on all sides, however this polyp was truly an early-stage colon cancer!
Food impaction in the esophagus is one of the emergency conditions that only gastroenterologists and emergency room doctors know about. The overall concept is simple: Soon-to-be patient eats a large quantity of food (most commonly meat), which gets stuck in the esophagus somewhere and then causes a blockage and prevents further swallowing. Patient experiences chest pain, … Read more
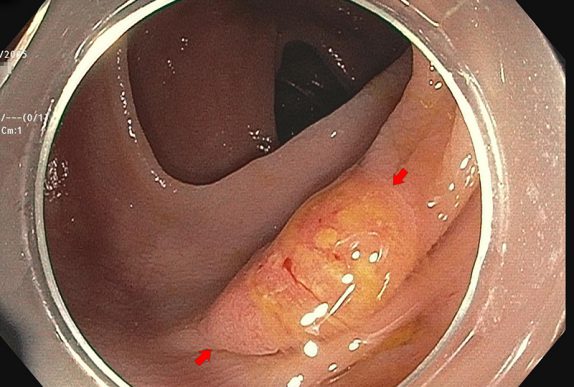
This lesion exhibits the "mucus cap" sign. There is a thick layer of mucus adherent to the polyp that remains attached even after washing with the water jet on the scope. The mucus cap sign is often seen with a particular type of polyp called a serrated polyp. These are often located in the right side of the colon, and are thought to be easier to miss on colonoscopy due to the flat nature of their growth. Unfortunately, they can still transform into colon cancer.
Dysphagia (trouble swallowing) can be caused by many different problems. A strictured or narrowed esophagus is one common cause, and is often related to excess acid exposure in the esophagus. Usually strictures happen at one discrete location in the esophagus (often the lower part closest to the stomach where acid reflux damage is the most pronounced).
So what are some take home points about meat intake in Crohn's disease? Red meat (beef, lamb, pork [yes pork too!]) can be though of as pro-inflammatory foods. It is reasonable to limit consumption of red meat to once or twice per week at most. Fish is probably a good alternative to red meat. These recommendations are based on very limited, low-quality data. Sometimes this is better than no data at all!
Subscribe To Our Newsletter!
Make sure to never miss a post by subscribing!