Part one of this topic can be found here.
Nonselective beta-blockers (NSBBs) are often indicated for prevention of variceal bleeding in cirrhotic patients. However, there has been a large amount of data in the past several years that have raised serious concerns over the safety and utility of beta-blockers in patients with more advanced cirrhosis. Patients with what is considered decompensated advanced cirrhosis have now been shown in numerous studies to have increased mortality when treated with beta-blockers. Interestingly, most of the original trials on beta-blockers from the 1980s-era excluded these patients from study, therefore this important caveat was never recognized back then!
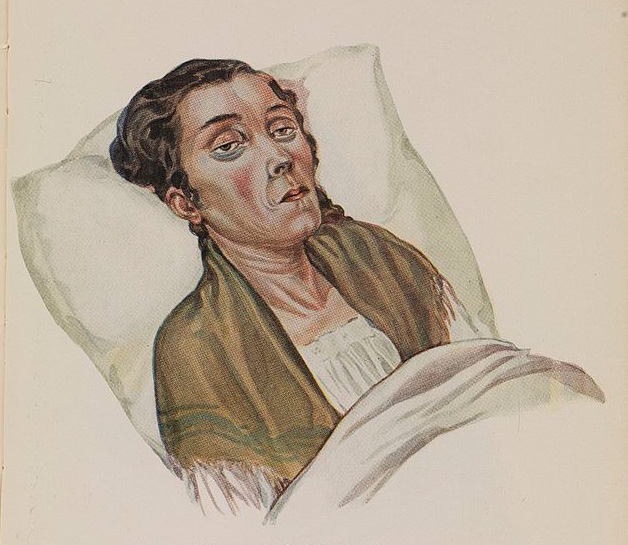
Beta-blockers blunt the sympathetic nervous system, which is a last-ditch survival mechanism to avoid systemic hypotension. Blocking this can lead to further decompensation in blood pressure and poor organ perfusion, especially of the kidneys. Hypotension, refractory ascites, and hepatorenal syndrome occurs, which is often the beginning of the death spiral of cirrhosis. In advanced decompensated cirrhosis, beta adrenergic tone is needed to survive, and blocking it is detrimental. To date, multiple high-quality studies have shown a dramatic increase in death among advanced patients who are treated with beta-blockers, with roughly a 20-45% absolute increase in mortality attributed to beta-blocker use. This is a huge effect!
Researchers have now been trying to define exactly when this advanced decompensated period occurs. There is still some debate in the area, but it is a pretty safe bet that the presence of diuretic-refractory ascites and/or the occurrence of spontaneous bacterial peritonitis (SBP) puts a patient into the advanced decompensated category. Here is a more comprehensive list of situations where beta-blockers are thought to be detrimental:
• refractory ascites
• systolic blood pressure < 100 mm Hg
• mean arterial pressure < 82 mm Hg
• acute kidney injury
• hepatorenal syndrome
• spontaneous bacterial peritonitis
• sepsis
• poor medical follow-up or poor compliance
In these patients, it has become my practice to stop any existing NSBB therapy (by slowly withdrawing the drugs over two weeks or so). In very decompensated patient with variceal bleeding, I would not start NSBB drugs for secondary prophylaxis either. Instead the focus should be on treating the variceal bleeding aggressively with endoscopic band ligation (tying off the varices with small rubber bands), or with placement of a TIPS (a shunt that reduces portal pressure dramatically). These data are practice-changing to me, and have broken a paradigm that has been in place in the literature for over thirty years.
If you enjoyed this article, sign up for our free newsletter and never miss a post!
The following are excellent references for further reading:
Ge PS, Runyon BA. The changing role of beta-blocker therapy in patients with cirrhosis. J Hepatol 2014;60:643-53.
Ge PS, Runyon BA. When should the beta-blocker window in cirrhosis close? Gastroenterology 2014;146:1597-9.
Mandorfer M, Bota S, Schwabl P, et al. Nonselective beta-blockers increase risk for hepatorenal syndrome and death in patients with cirrhosis and spontaneous bacterial peritonitis. Gastroenterology 2014;146:1680-90.
Image via Wellcome Library, London.