Nasogastric tubes (NGTs) are used to access the stomach either for drainage, or to provide access for feeding when a patient is unable to eat for various reasons. As the name implies, the tube enters the nose, and the tip sits in the stomach. Most of the time, the tubes can be easily passed “blindly” at the bedside without any special equipment or sedation. However, every once in a while, the tube cannot be passed for various reasons, often related to problems in the esophagus such as strictures, tumors, or large hiatal hernias.
In these cases, blind passage of the tube is often impossible, and repeated attempts can be dangerous. Often endoscopy is needed to successfully place the tube into the stomach. This is usually a simple task, but can also become quite difficult since the tip of the NGT doesn’t always go where you want it to go. Also, getting the tube where you want it may be easy, however keeping it there while you remove the scope may be very hard because the friction between the tube and the scope drags the tube back out!
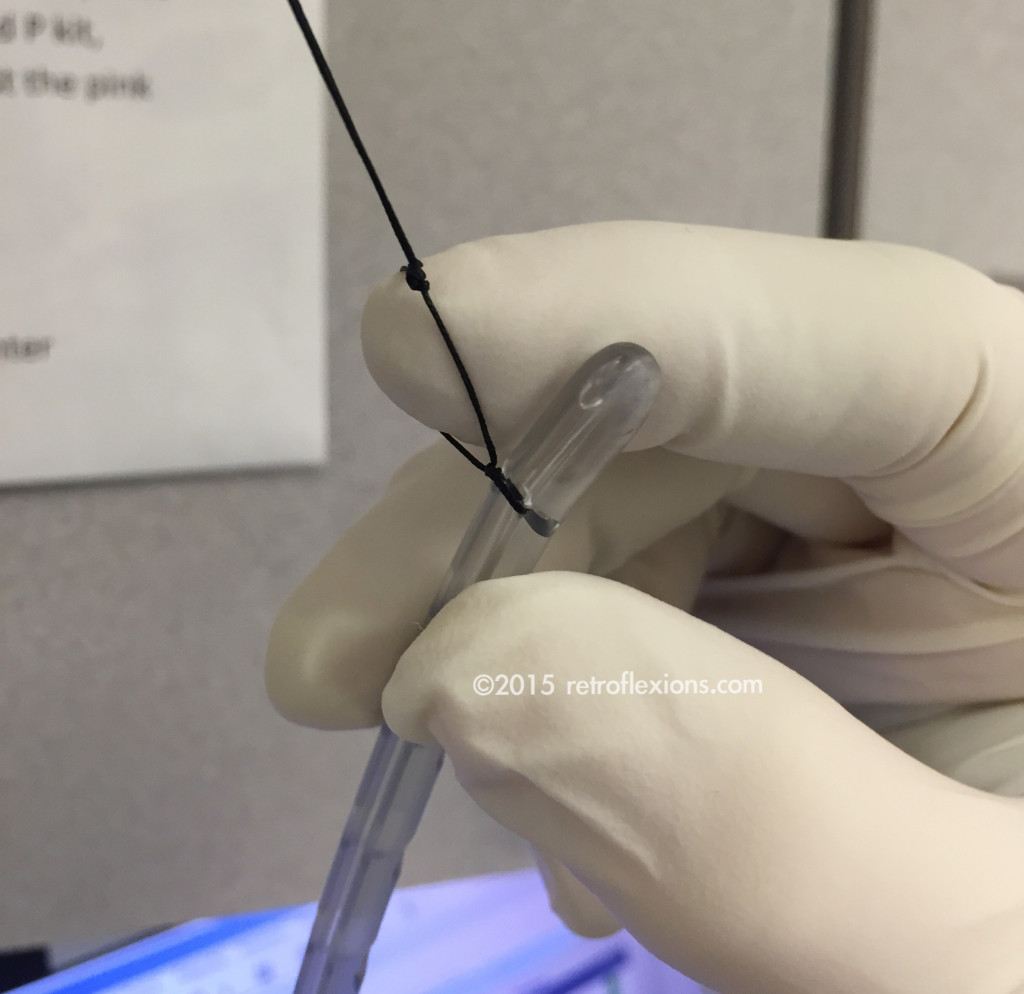
After tying the suture around the tip of the tube, form and tie a loop by using an assistant’s fingertip as shown above.
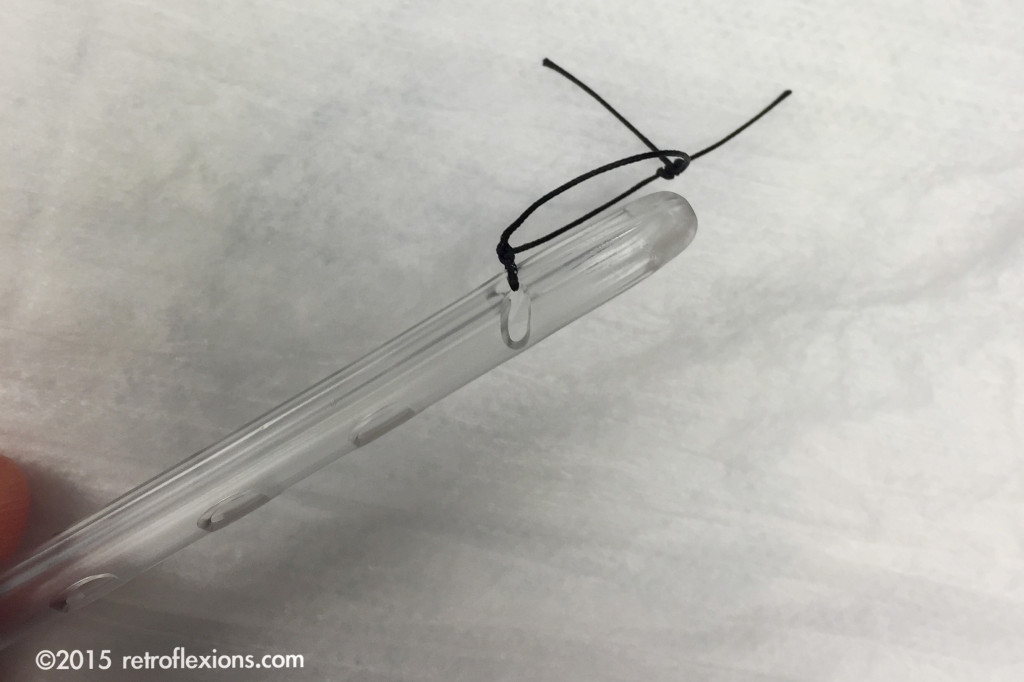
Here is the tube ready to be placed, with a small loop at the tip used to grasp and/or fix the tube once placed.
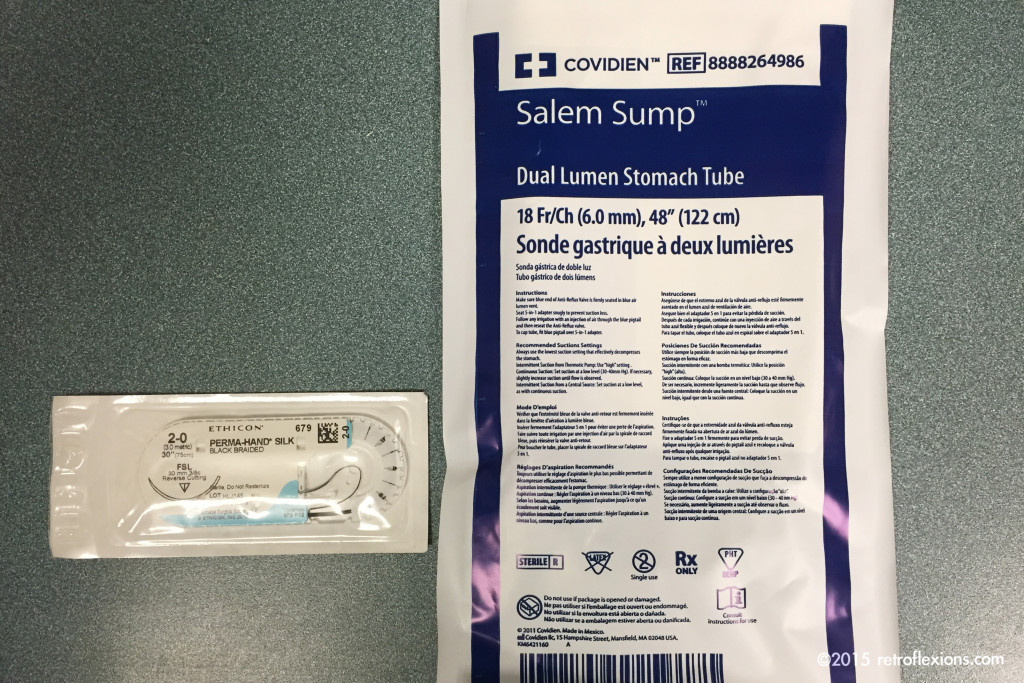
One technique that is helpful is to tie a suture (with a small loop in it) to the very end of the NGT. Once passed via the nose into the esophagus or pharynx, this suture can be used to grasp the tube with forceps and direct the tip wherever you need it to go. It also allows the application of clips to fix the tube in place (temporarily, in the case of a jejunal tube) in the small bowel which can prevent the tube from migrating out when you remove the scope. Sometimes I will even put a stiff guide wire through the lumen of the tube (using plenty of lube) to stabilize it while the scope is removed. Then the guide wire is removed afterwards. For an added margin of safety, if the tube placement was challenging I will usually check an X-ray afterwards to confirm the location of the tip before using the tube.
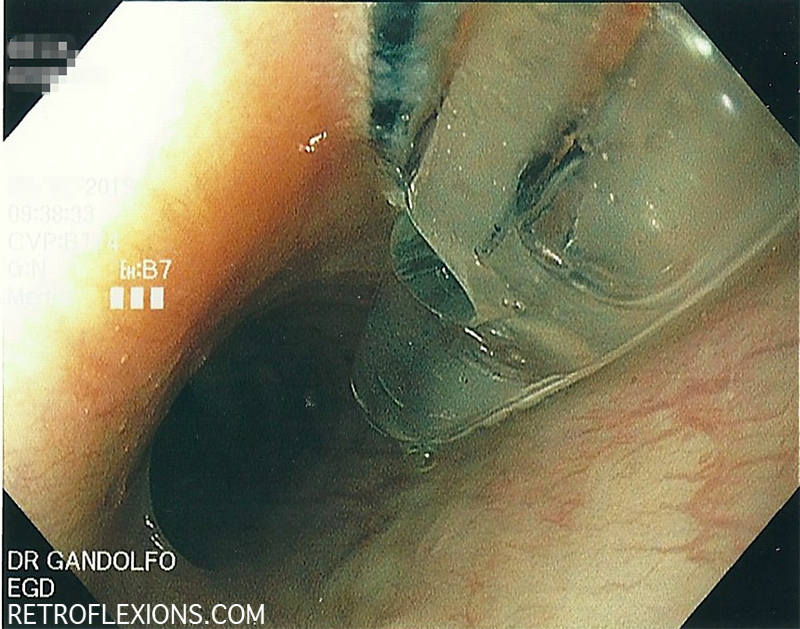
Tube with suture-loop in the esophagus. In this case, the patient had an esophageal ring that was preventing blind placement of the NGT.
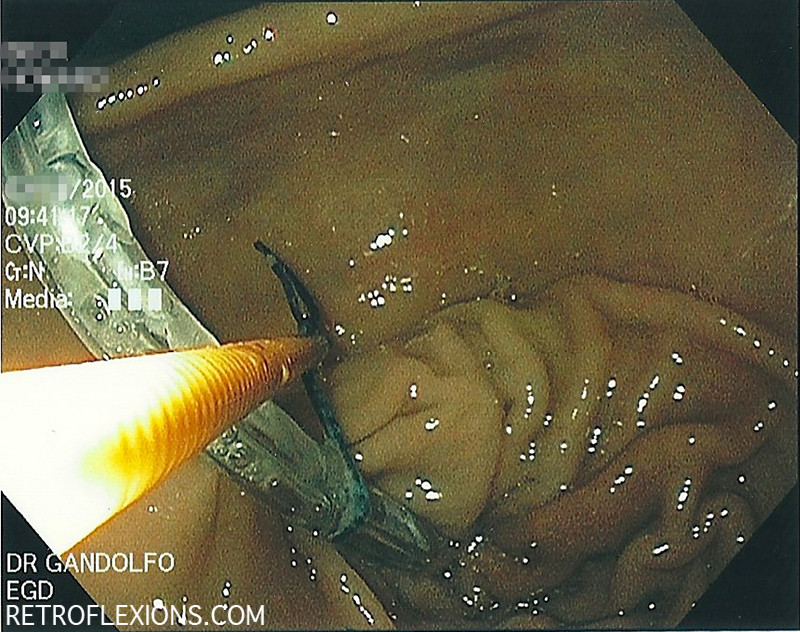
A standard biopsy forceps (orange-colored instrument) is used to grasp the suture loop to drag the tube into the stomach.
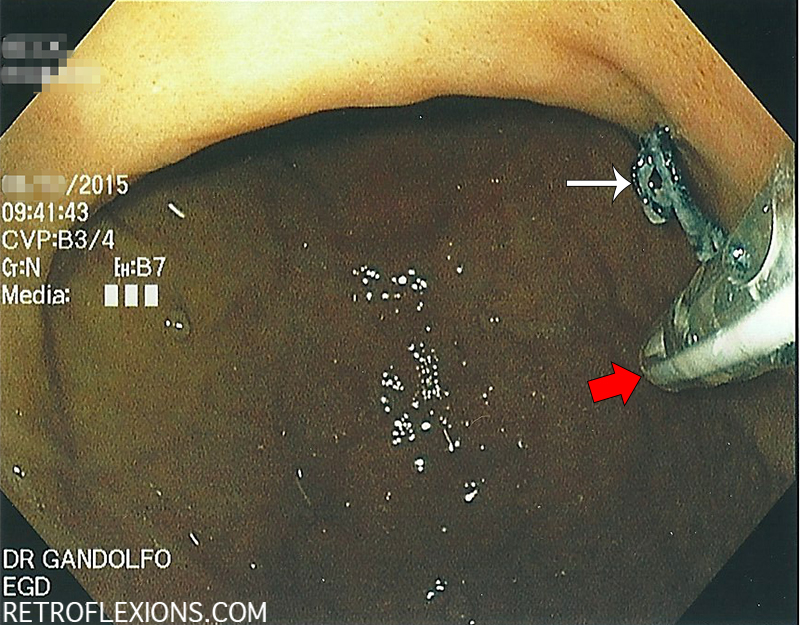
Another picture of the tube placement showing the tube (red arrow) and the suture (white arrow). In this case, the tube was not fixed in place using clips.
Endoscopic tube placement is safe and effective when bedside placement is not possible. Other methods, such as radiologic tube placement are also effective, and the choice should be made based on local expertise.
If you enjoyed this article, sign up for our free newsletter and never miss a post!
Reference:
Gerritsen A, van der Poel MJ, de Rooij T, et al. Systematic review on bedside electromagnetic-guided, endoscopic, and fluoroscopic placement of nasoenteral feeding tubes. Gastrointest Endosc 2015;81:836-847.