“Are you still taking lasix?” I asked the patient. He was new to the office, here for a routine post-hospital follow up visit after recently being admitted for decompensated cirrhosis with ascites and fluid overload. His dose of lasix was resumed prior to discharge, and he was supposed to be taking 80 mg daily.
“I don’t take lasix,” he replied. “My doctor took me off that.”
“But you wrote down ‘furosemide’ on your med sheet today…I’m confused,” I said, holding the handwritten list of ten medications that the patient’s wife filled out only a few minutes prior in the waiting room. The list was copied from the printed discharge instructions from the hospital.
“Of course, I’ve been taking furosemide forever,” he said with a funny look on his face. “I started taking it again after I left the hospital, one pill every morning.”
“I’m sorry, I should have mentioned that lasix and furosemide are the same thing,” I said. Patients (and doctors) get mixed up with trade and generic names for drugs all the time, so I understood the confusion. “Now, how many milligrams are you taking again?”
“I don’t know how many milligrams. It’s one pill, a little white one,” he said while holding up his thumb and pointer finger in a pinching gesture to show me just how little the white pill was. “It’s the same thing I was taking before I went in to the hospital.” At this point, I could tell he wasn’t sure I was listening to him.
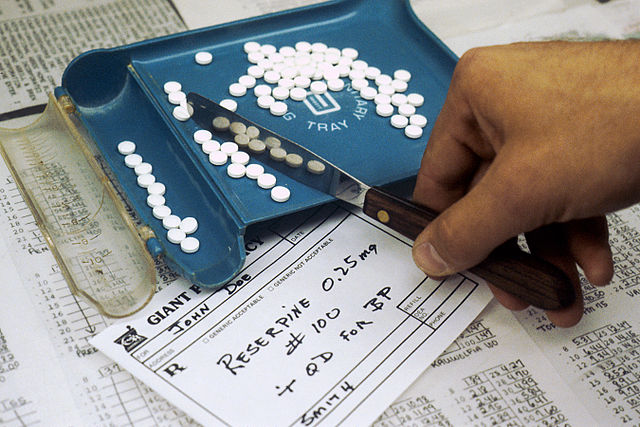
Furosemide (AKA lasix) is a diuretic medication, and typically comes in 20 mg and 40 mg tablets. In reality, he was getting 80 mg in the hospital to get rid of the excess fluid in his body. One of the reasons he ended up in the hospital in the first place is because the dose of lasix was probably not enough at home. Now it seems that the same home dose was resumed. I assume he is taking the 40 mg dose since that is the more common tablet out there. I am always uncomfortable assuming what medications and doses my patients are taking; I would rather know them for sure. When I tell him to take two pills per day starting tomorrow, is he going to be taking 40 mg or 80 mg daily?
What I usually do in these circumstances is give the patient a new prescription for the appropriate drug and dose that he should be taking. I then ask him to put his old versions of the medication in a bag and either throw them out or bring them to the next visit so I can sort through them and try to make sense out of it all. Or I have the patient or a family member call me from home and read exactly what it says on their pill bottle. Luckily lasix is cheap, however asking a patient to get a new prescription for an expensive drug or a controlled substance is not always easy.
Want to be a better patient? Know what medications you are taking. Keep a list with you all the time, and write the date the list was updated on the top. When the list gets sloppy from cross outs and medication changes, make a new one. Write or type them out in the following way:
Drug name: dose with appropriate units (e.g., milligrams), how many times per day that dose is taken.
I don’t need to know how many pills you take to arrive at the dose you are taking. Pills come in different sizes and shapes and there are a lot of little white pills out there! It’s also not terribly important to know what time you take the pills, or if you take them with food or not. Sometimes I do need to know those details and will ask specifically, however if I am just trying to understand what medications are circulating in your bloodstream on a daily basis, the minimal information I need is the drug name and dose per day.
From an efficiency standpoint, if we have an average of 10-15 minutes of doctor-patient face time for your appointment that day, and we spend 5 minutes trying to figure out a basic thing like what medications and doses you are taking, then we just wasted about half of our time. A simple pre-made list would have solved the problem, and we would both know for sure what medications you are taking. That time we just saved can now be applied to something more important, like talking about diet, or education about the disease we are treating, or some new symptom you are having.
Remember, you are putting this stuff into your body…you should at least know what it is called!
If you enjoyed this article, sign up for our free newsletter and never miss a post!