An angiodysplasia is a type of vascular malformation that is commonly found throughout the gastrointestinal tract, and fairly often in the right colon. These lesions can be described as thin-walled, fragile, superficial abnormal “tangles” of small blood vessels that have a propensity to bleed, especially in patients who take blood thinning medications. In a patient with anemia or bleeding, we usually treat these lesions with some type of cautery, most commonly argon plasma coagulation (APC). Other terms used for angiodysplasia include arteriovenous malformation (AVM), angioectasia, telangiectasia. (These terms actually all mean slightly different things, but let’s not get into that now.)
When treating angiodysplasia in the right colon, especially in the thin-walled cecum, it is important to use a minimal amount of APC, delivered in short bursts at low flow settings. The concern is that immediate, or more often late, damage can occur to the bowel wall leading to perforation. One useful technique to minimize the risk of perforation when treating large angiodysplastic lesions (let’s arbitrarily define large as greater than 10-mm in diameter) is to first inject saline under the lesion to lift it up and away from the deeper layer of bowel wall. Yes, this is exactly like the way we treat big polyps, so it is already a skill that most gastroenterologists have.
Although this angiodysplasia was not that large (maybe just 10-mm in the largest dimension), this patient was taking dual antiplatelet therapy, and needed to go on full-dose anticoagulation right after the procedure. Since the lesion was in the cecum, it was a good candidate for lifting prior to cautery.
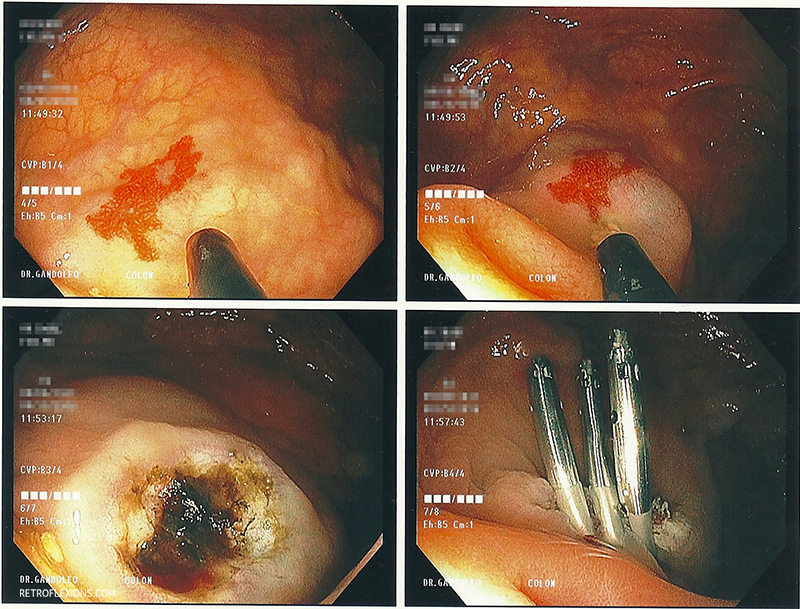
Treatment of cecal angiodysplasia with APC: The lesion is lifted with submucosal injection of saline (the ileocecal valve can be seen in the second picture). After injection, APC is used to ablate the lesion. A few clips were placed to prevent delayed bleeding since the patient needed to remain on multiple blood-thinning agents.
For an excellent review of gastrointestinal angiodysplasia, including theories on why they form, see the following reference:
Sami SS, Al-Araji SA, et al. Review article: gastrointestinal angiodysplasia-pathogenesis, diagnosis, and management. Aliment Pharmacol Ther 2014;39:15-34.