Cirrhosis is the final common stage of most types of chronic liver disease, and appears as “scarring” of the liver tissue under the microscope. The liver becomes firm, and instead of blood flowing easily through the organ on the way back to the heart there is a high level of resistance to blood flow through the hard nodular liver.
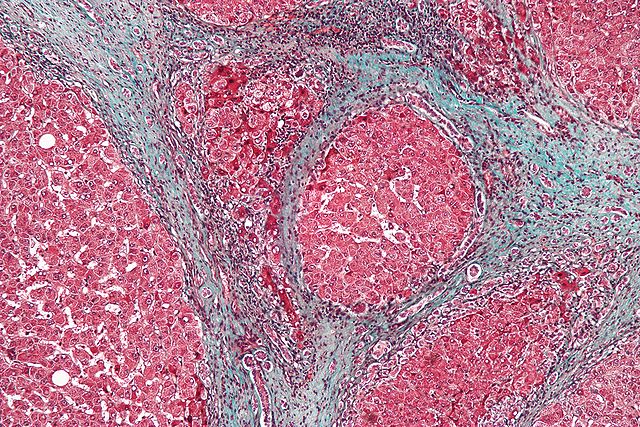
Microscopic image of a liver biopsy from a cirrhotic liver (trichrome stain). The blue color highlights fibrous connective tissue, which forms band-like scars in between the liver tissue (which stains red).
Eventually portal hypertension occurs, which can be thought of as a high pressure in the portal vein that feeds into the liver from the digestive system. When high pressure exists in any system, the pressure always wants to equalize, and the body will find ways of growing “new” veins that bypass the liver and allow the high pressure to be relieved. These abnormal veins are called varices, and most commonly form in the esophagus, but also in many other places. Varices can rupture without pain or any warning whatsoever, causing rapid life-threatening bleeding.
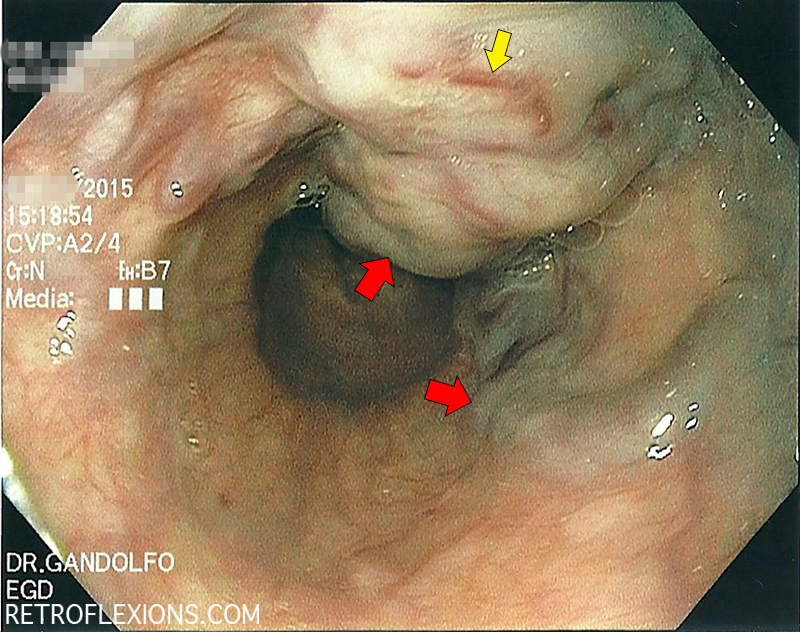
Endoscopic view of large esophageal varices. The bluish-colored protuberant columns are varices (red arrows). The yellow arrow shows a “red wale sign” which is a marker of high pressure inside the varix and portends a high risk of bleeding.
Portal hypertension is also the pathway for most of the major complications from cirrhosis, including ascites, variceal bleeding, kidney failure, and hepatic encephalopathy. Treating portal hypertension with nonselective beta-blockers (NSBBs, e.g., propranolol, carvedilol) has been shown to decrease variceal bleeding and improve survival in some patients with cirrhosis and varices.
Here is a quick review of the current indications for nonselective beta-blockers in cirrhosis:
✓ The prevention of the first episode of bleeding in patients with large varices
✓ The prevention of another episode of bleeding in patients with a history of variceal bleeding
✓ A cardiac indication for beta-blockers (e.g., heart failure, etc.) in a patient with early cirrhosis
How do beta-blockers work in patient’s with cirrhosis?
Cirrhosis is characterized by systemic vasodilation and decreased peripheral arterial resistance which (if not opposed) will cause low blood pressure and shock. Therefore, to prevent this, cardiac output and heart rate is usually increased in patients with advanced cirrhosis. The body activates other compensatory mechanisms such as the renin-angiotensin-aldosterone system to retain salt and water due to a decrease in the effective arterial pressure. The beta adrenergic system (sympathetic nervous system) is also used as a compensatory mechanism to keep blood pressure up and allow the vital organs to be perfused with adequate blood flow. Nonselective beta-blockers work here to both decrease cardiac output (beta-1 effect), and decrease portal blood flow by constricting the splanchnic (gut) blood vessels (beta-2 effect). This decreases the blood flow in the portal system and therefore decreases the pressure inside the varices, lessening the chance that a varix will rupture and bleed.
In properly selected patients, the effect of beta-blockers on preventing variceal bleeding is excellent. Many studies have shown large decreases in the rates of bleeding and death over many years if NSBBs are used appropriately. One important point, is that NSBB therapy has to be adjusted properly to have any clinical effect. Often patients are put on these drugs at the lowest starting dose and just left at that dose forever. However, all of the studies that showed a benefit of NSBBs on variceal bleeding did the following at each visit:
Adjust the dose of the beta-blocker to result in a 20-25% reduction in resting heart rate (from the pre-drug baseline), or to a goal heart rate of 55 beats per minute as blood pressure and side-effects allow.
However, recently there has been a flurry of new data regarding the use of NSBBs in patients with decompensated advanced cirrhosis that show increased mortality associated with these drugs. This is practice-changing information and will be covered in a future post…
If you enjoyed this article, sign up for our free newsletter and never miss a post!
[Update: here is part two…Beta-blockers: friend or foe?]
Reference:
Ge PS, Runyon BA. The changing role of beta-blocker therapy in patients with cirrhosis. J Hepatol 2014;60:643-53.
Liver histology image by Nephron
