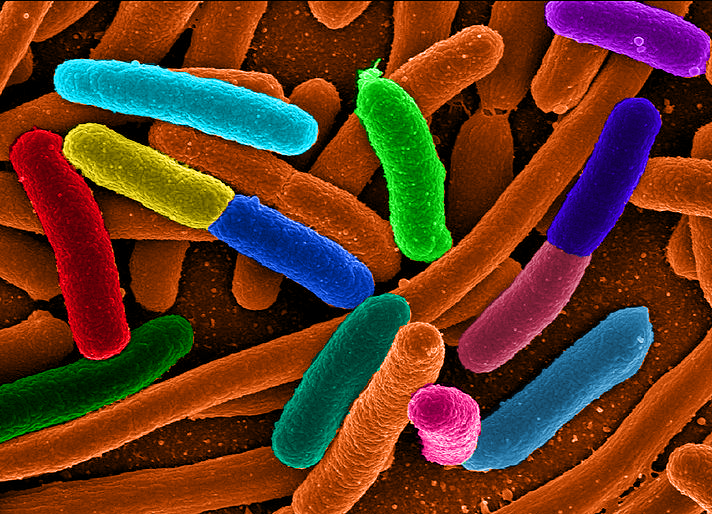
There have been a lot of reports surfacing recently regarding strange infections associated with endoscopy. At the time of publication of this article, there have been about 135 confirmed cases of infection with Carbepenem-resistant Enterobacteriaceae (CRE), which are mainly multi-drug resistant E. coli and Klebsialla species. These infections are relatively rare in general, and are very problematic because the bacteria are resistant to almost all current antibiotics.
 First off, I must clarify that so far, all cases of endoscopy-associated CRE infections have been associated with a special type of scope used for a procedure called ERCP (endoscopic retrograde cholangiopancreatography). ERCP is an indispensable, often life-saving, procedure to relieve obstructions and provide drainage of the bile duct. Gallstones can become trapped in the duct causing pancreatitis, severe pain, or a deadly infection known as cholangitis, or the duct can become blocked from various types of tumors. There are also many other indications for ERCP that are less common than stones or cancer. ERCP is a very specific procedure for a very specific group of problems, and when needed often nothing else will do. As an analogy, one could probably figure out a way to drive a screw into a piece of wood with a pair of pliers, or even a hammer, but the end result will never be as good as if you just used a screwdriver.
First off, I must clarify that so far, all cases of endoscopy-associated CRE infections have been associated with a special type of scope used for a procedure called ERCP (endoscopic retrograde cholangiopancreatography). ERCP is an indispensable, often life-saving, procedure to relieve obstructions and provide drainage of the bile duct. Gallstones can become trapped in the duct causing pancreatitis, severe pain, or a deadly infection known as cholangitis, or the duct can become blocked from various types of tumors. There are also many other indications for ERCP that are less common than stones or cancer. ERCP is a very specific procedure for a very specific group of problems, and when needed often nothing else will do. As an analogy, one could probably figure out a way to drive a screw into a piece of wood with a pair of pliers, or even a hammer, but the end result will never be as good as if you just used a screwdriver.
The special scope used for ERCP is called a duodenoscope, also known as a side-viewing scope. One of the things that makes a duodenoscope different from other scopes is the presence of a small metal tab known as an elevator at the tip of the scope. The elevator is crucial to a successful ERCP as it is used to change the angle of the instrument used to access the bile duct. The problem is that the elevator mechanism itself has tiny moving metal parts that may still harbor bacteria after scope reprocessing, despite following proper scope cleaning and disinfection protocol.
There have not been any reports that I am aware of where CRE infections were contracted from standard scopes used for routine upper endoscopy or colonoscopy. Recently, I have had patients asking if they should cancel their scheduled procedures because of the news reports about these infections. While very concerning in general, there is virtually no risk of getting this infection from a routine endoscopy or colonoscopy if the scopes were cleaned correctly.
The FDA has reported 135 such cases of CRE infections associated with ERCP over a two year period, mostly as outbreaks at a few different centers. They estimate that about one million ERCPs have been done nationwide in that time period. We can be sure that not all cases of infection have been identified or reported, so the “135 patients” number is probably lower than the true number of cases. So what is the actual risk? If we assume that there are probably closer to 200 cases of CRE infection from scopes out there, then 200 divided by 1,000,000 is 0.0002. Multiplying by 100, we get 0.02%, the actual risk of getting a CRE infection if you have had an ERCP. This translates to two patients out of every ten-thousand who have an ERCP.
So is this concerning? Sure it is. No doctor wants to think that the procedure they did to help someone ended up causing a bigger problem. And keep in mind that we are just talking about infections with CRE, a bacteria that is very rare and difficult to treat, therefore each case identified sends up a red flag. How many people are infected with more common and treatable bacteria from these scopes?
I am sure that eventually this issue will be overcome and there will have to be new cleaning protocols developed for these scopes. However what about the whole issue with the growing number of bacteria that are resistant to all antibiotics? To me, that is the more concerning issue. The overuse and inappropriate use of antibiotics over many years have produced these so-called “superbugs.” That is something to worry about more that a 0.02% chance of a scope-related infection.
As stated above, ERCP is usually indicated for several potentially life-threatening conditions that affect the biliary system and pancreas. As with anything in medicine, the decision to perform an invasive test should take into account all the risks, benefits, and alternatives before proceeding. Would the patient be better served with a non-invasive imaging test such as a MRCP or CT scan? What about endoscopic ultrasound? With the continued improvement and validation of advanced imaging techniques, the need for ERCP is now usually reserved for intervention (stents, stone extraction, biopsy, etc.), not merely diagnosis. If an ERCP is truly indicated, then the risks of not performing the test are hundreds of times greater than the risk of contracting one of these rare infections. As of now, while still concerning, actually contracting a CRE infection should be the absolute lowest item on the list of potential complications and issues that either the doctor or patient should worry about.
If you enjoyed this article, sign up for our free newsletter and never miss a post!
References:
Centers for Disease Control and Prevention (CDC). Notes from the field: New Delhi metallo-β-lactamase–producing Escherichia coli associated with endoscopic retrograde cholangiopancreatography — Illinois, 2013. MMWR Morb Mortal Wkly Rep 2014 Jan 3; 62:1051.
FDA bulletin: http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm434871.htm
Muscarella LF. Risk of transmission of carbapenem-resistant Enterobacteriaceae and related “superbugs” during gastrointestinal endoscopy. World J Gastrointest Endosc 2014;6:457-74.
