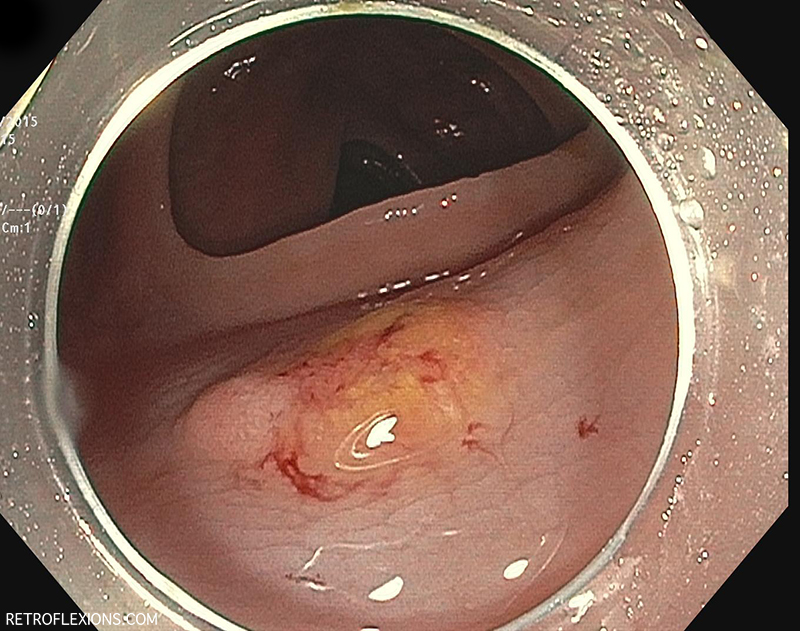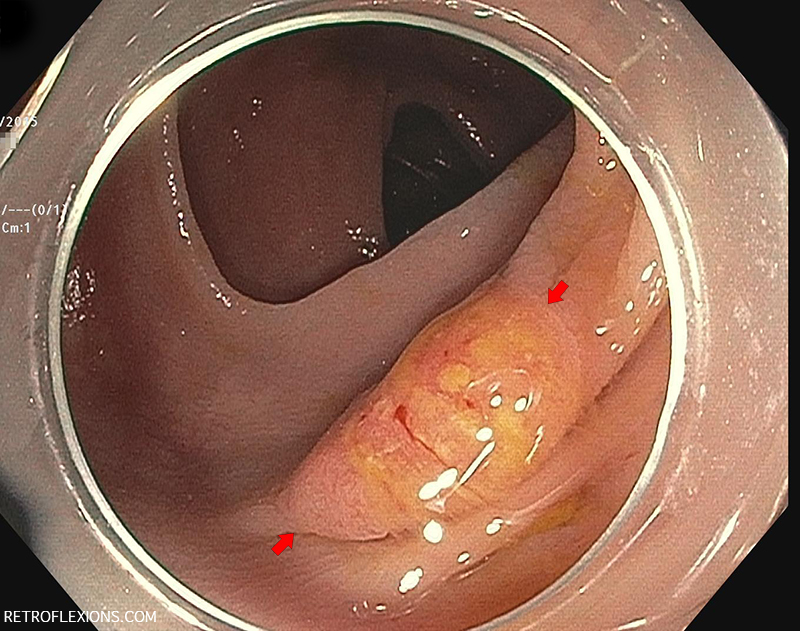
Flat slightly-ulcerated lesion (between red arrows) in the transverse colon showing the mucus cap sign. The yellow material is adherent mucus.
This lesion was picked up in a patient during a colonoscopy done to investigate the cause of chronic diarrhea. It is an incidental finding.
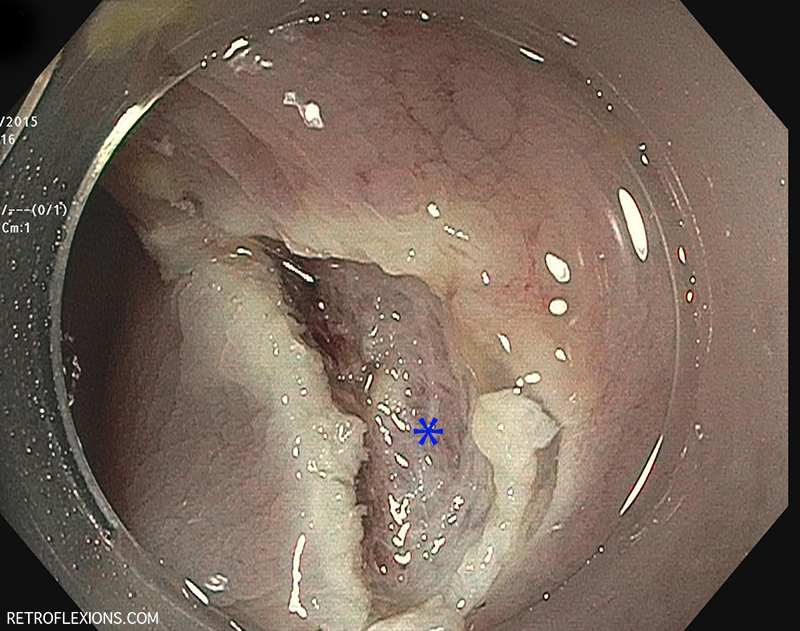
This lesion exhibits the “mucus cap” sign. There is a thick layer of mucus adherent to the polyp that remains attached even after washing with the water jet on the scope. The mucus cap sign is often seen with a particular type of polyp called a serrated polyp. These are often located in the right side of the colon, and are thought to be easier to miss on colonoscopy due to the flat nature of their growth. Unfortunately, they can still transform into colon cancer. This goes to show that: A) Excellent prep is very important to a high-quality colonoscopy when the goal is preventing colon cancer; and B) When an area in the colon seems to have mucus attached, it is a good idea to go investigate that area more thoroughly.
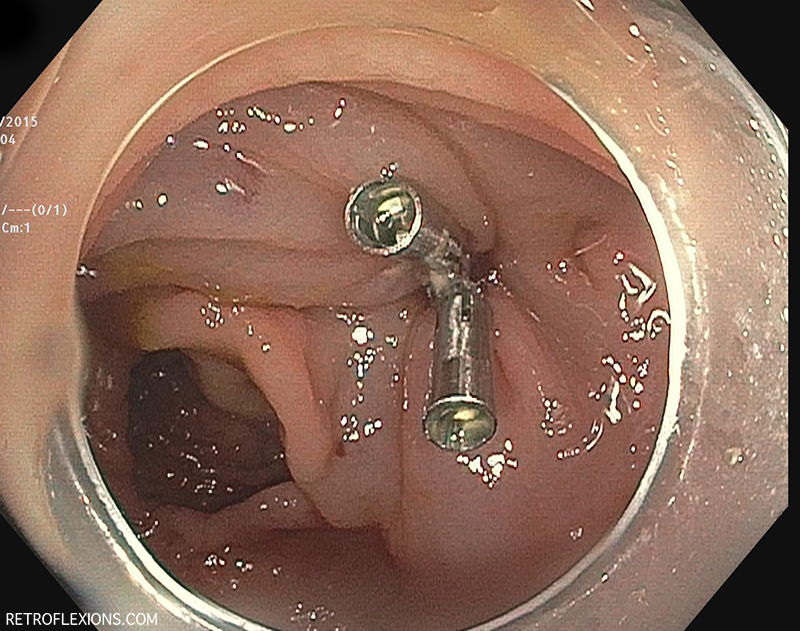
Speaking of caps–if you notice, there is a clear plastic cap on the tip of the scope that you can see in the endoscopic images. This cap is designed to improve visualization by allowing the endoscopist to push folds out of the way and inspect behind them. It is also useful for taking out certain polyps, as it allows the operator to get the tip of the scope very close to something without that something touching the lens and preventing visualization. There is some data that using a short cap on the scope may very slightly improve polyp detection. The effect is quite small however, and there was no increase in the detection of adenomas (pre-cancerous polyps), which are the polyps that we really care about finding.
This lesion was removed using standard endoscopic mucosal resection technique. About 20 cc of saline was injected to give a generous lift. The lesion was then encircled with a stiff snare and removed using cautery in one piece. The base was then inspected and looked good: no sign of bleeding, perforation, or residual polyp. Next, the mucosal defect was approximated with two clips.
Please see Flat “polyp” resection (part two), to review the pathology findings and management strategies of this interesting lesion.
If you enjoyed this article, sign up for our free newsletter and never miss a post!
References:
Pereyra L, Gomez EJ, Gonzalez R, et al. Finding sessile serrated adenomas: is it possible to identify them during conventional colonoscopy? Dig Dis Sci 2014;59:3021-6.
Ng SC, Tsoi KK, Hirai HW, et al. The efficacy of cap-assisted colonoscopy in polyp detection and cecal intubation: a meta-analysis of randomized controlled trials. Am J Gastroenterol 2012;107:1165-1173.
Saito S, Tajiri H, Ikegami M. Serrated polyps of the colon and rectum: endoscopic features including image enhanced endoscopy. World J Gastrointestinal Endosc 2015;7:860-71.